Traumatic Brain Injury
Traumatic brain injury (TBI) occurs when a person experiences a violent blow or jolt to the head or body resulting from a car accident, a fall, a sports injury, or an assault. The blow causes the head and brain to move rapidly back and forth, damaging brain cells and causing injuries that range from mild to life-threatening. There are three main types of TBI: mild TBI (also known as concussion), moderate TBI, and severe TBI.
Those at high risk for traumatic brain injury include children (especially newborns and young children), young adults, adults age 60 or over, and males of any age group. Members of the military, especially those who served in Operation Enduring Freedom and Operation Iraqi Freedom are also at higher risk (approximately 20% of veterans from these conflicts suffered some sort of TBI).
Symptoms of traumatic brain injury may appear immediately after the traumatic event, or they can appear days or weeks later. These may include:
Headache
· Nausea and vomiting
· Fatigue or drowsiness
· Problems with speech
· Dizziness or loss of balance
· Sensitivity to light or sound
· Loss of consciousness ranging from a few seconds to a few minutes or hours
· Feeling dazed, confused, or disoriented
· Convulsions or seizures
· Dilation of the pupils
· Memory or concentration problems
· Mood changes or mood swings
· Feeling depressed or anxious
· Changes in sleeping patterns
· Loss of coordination
· Agitation or unusual behavior
Traumatic brain injury can lead to or exacerbate mental health symptoms, so it’s important to let your counselor know if you have ever experienced a TBI. Survivors of TBI may struggle with depression, personality changes, memory loss, impulsivity, irritability, and cognitive or language difficulties. They may also have co-occurring conditions such as post-traumatic stress disorder (PTSD).
Treatment for TBI depends on the severity of the injury and its effects. A person with a moderate or severe TBI may need to see several health care providers, including doctors, mental health counselors or psychologists, speech and occupational therapists, and other professionals. Treatment may include rest, surgery, medication, and rehabilitation therapy. Neurofeedback is a natural, non-invasive treatment for TBI that may help improve functioning. At the ADHD and Neurofeedback center, we provide counseling and therapy for clients with a history of TBI.
Neurofeedback Individual Therapy in Houston, Kemah, the Woodlands areas, and Utah County
Our clinicians support and assist clients in connecting with their authentic selves and learn to be their best selves. Also, behaviors will be evaluated that are not currently working for them. We utilize the Neurofeedback therapy modality. The neurofeedback modality is research-based and shows success based on the particular issues and the client.
Therapy Options for You
Our greatest desire at ADHD and Neurofeedback is to help each feel comfortable and hopeful about their therapy process. Please feel free to contact us with any questions or concerns. We also offer a free consultation to help assess how therapy can benefit you and help you to feel peace and happiness again. We provide Neurofeedback therapy services in Houston, Kemah, the Woodlands areas, and Utah County.
How can Neurofeedback help with TBI?
Getting Started with EEG Neurofeedback (Second). (2019, January 22). W. W. Norton & Company.
(Getting Started With EEG Neurofeedback, 2019)
How can Neurofeedback help with Traumatic Brain Injury?
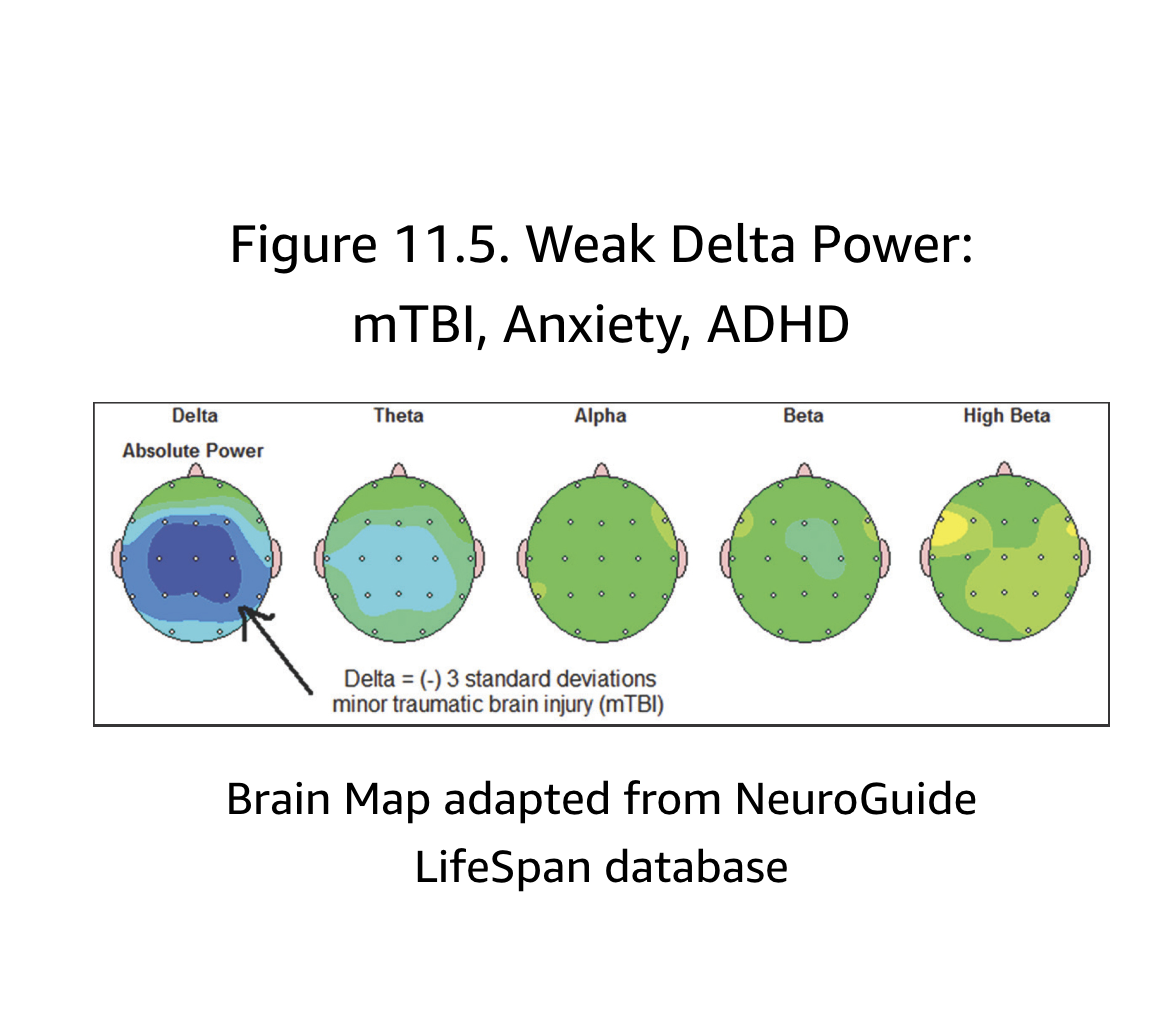
Neurofeedback is a viable treatment option for sufferers of TBI because it can target the specific part of the brain that has been injured. In the part of the brain that has been damaged, Delta and Theta brain waves rush to the area; however, they often become locked, thus preventing growth in the area.
Neurofeedback can pinpoint these areas in the brain and provide direct feedback, creating more optimal brain waves in the damaged area of the brain.
A 2011 study found that the use of neurofeedback training in “6 traumatic brain injury patients, all-sustaining their injuries by a car accident. Cognitive difficulties were observed as the main area of concern, with QEEG assessment identifying a predominance of frontal brain waves in the patients. Following 20 sessions of neurofeedback (twice per week, 40 minutes duration), 5 of the 6 patients were able to return to normal education, and all reported improvements concerning mood, quality of sleep, and cognitive abilities” (Zorcec 2011, see Research page for more).